"News with equal focus on each person"
| 6 January 2005 | Archive | Subscribe for free by E-mail
or |
|
Vampires In Our MidstBy Larry Baum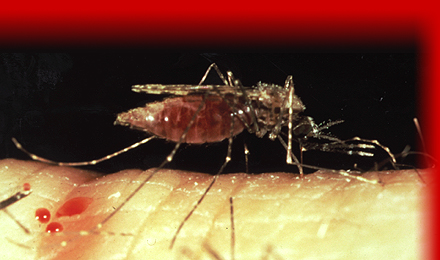 Mosquitoes transmit the malaria parasite to humans.
To keep rebellious military units in line, the Roman Empire used a vicious practice called decimation: killing every tenth person. In the first half of the twentieth century, malaria decimated the human race, causing approximately 10% of all deaths. Mosquito control measures and antimalaria drugs reduced the death rate in later decades, but currently 1-3 million people still die and about a third to a half of a billion become ill from malaria each year. Malaria is caused by the protozoan parasite, Plasmodium. The most virulent species of this single-celled organism is P. falciparum, which causes 80% of cases and about 90% of deaths. Other species that cause malaria are P. vivax, P. ovale, and P. malariae. Plasmodium leads a complex lifestyle, changing homes and forms several times. The vectors for human malarial parasite are certain species of Anopheles mosquito. Infected female mosquitoes carry Plasmodium sporozoites in their salivary glands. If they bite a person, which they usually do starting at dusk and during the night, the sporozoites enter the person's body via the mosquito's saliva and migrate to the liver, where they multiply within liver cells. They then turn into merozoites, which enter red blood cells. There they multiply further, periodically breaking out of the red blood cells. The classical description of waves of fever coming every three or four days arises from simultaneous waves of merozoites breaking out of red blood cells. The parasite is relatively protected from attack by the body's immune system because it stays inside liver and blood cells. However, circulating infected blood cells are killed in the spleen. To avoid this fate, the parasite produces certain surface proteins which infected blood cells express on their cell surface, causing the blood cells to stick to the walls of blood vessels. These surface proteins are highly variable and cannot serve as a reliable target for the immune system. The stickiness of the red blood cells is particularly pronounced in Plasmodium falciparum malaria, and this is the main factor giving rise to hemorrhagic complications of malaria. Some merozoites turn into male and female gametocytes. If a mosquito bites the infected person and picks up gametocytes with the blood, fertilization occurs in the mosquito's gut, new sporozoites develop, and the sporozoites travel to the mosquito's salivary gland, completing the cycle. The classic clinical course of malaria consists of bouts of fever accompanied by other symptoms and alternating with periods of freedom from any feeling of illness. The intermittent type of fever is usually absent at the beginning of the disease, when headache, malaise, fatigue, nausea, muscular pains, slight diarrhoea and slight increase of body temperature are the predominant and vague symptoms, often mistaken for influenza or a gastrointestinal infection. Most severe forms of the disease result in organ failure, delirium, impaired consciousness and generalized convulsions, followed by persistent coma and death. Young children are especially vulnerable. Pregnant women are especially attractive to the mosquitoes, and because parasites can be transmitted from mother to child before and/or during birth, malaria in pregnant women is an important cause of still births and infant mortality.  Copyright: WHO/Pierre Virot
Baby in advanced stage of malaria at Garki General Hospital in Abuja, Nigeria
Because mosquitoes carry the malaria parasite, areas where Anopheles mosquitoes live are vulnerable to malaria. Over 2 billion people live in these areas. The vast number of malaria deaths occur among young children in Africa, especially in remote rural areas with poor access to health services. Other high risk groups include women during pregnancy, and non-immune travellers, refugees, displaced persons, or labor forces entering into endemic areas. |
(continued) Malaria can be fought by preventing mosquitoes from biting people. Efforts to eradicate malaria by attacking mosquitos have been successful in some areas. Malaria was once common in the United States and southern Europe, but the draining of wetland breeding grounds and better sanitation eliminated it from affluent regions. Malaria was eliminated from the northern parts of the USA in the early twentieth century, and the use of the pesticide DDT during the 1950s eliminated it from the south. Use of mosquito repellents such as DEET, and mosquito nets and screens, can reduce the transmission of malaria. Insecticide-treated nets (ITNs) are now favored for their effectiveness and low cost. Drugs can also be used to prevent or treat malaria. Since the 17th century, quinine has been commonly used for prevention. In the 20th century, conventional antimalarial drugs, such as chloroquine, sulfadoxine–pyrimethamine (SP), and amodiaquine, have been effective. But inappropriate durg use has contributed to the evolution of resistance in malaria parasites: antimalarial drugs were deployed widely and were always used alone, introduced in sequence, and continued to be used despite unacceptably high levels of resistance. Over the past decade, artemisinin drugs has been increasingly widely used. These drugs work quickly, and with relatively few side effects. A variety of other drugs and vaccinces are under development or testing. Interactions between malaria and other diseases or environmental factors can affect risk of disease and death. Malnutrition can increase the severity of malaria. HIV increases severity of malaria in pregnant women, and vice versa. Malaria has economic consequences. A 2002 study by economist Jeffrey Sachs at Harvard's Center for International Development found that countries with high exposure to Plasmodium falciparum malaria in 1965 had annual economic growth rates that were 1.3% lower than other countries over the period 1965-1990, even after controlling for levels of human capital, life expectancy, initial income, and macroeconomic policy indicators of various kinds as well as geographical factors such as tropical location that could be simultaneously influencing malaria and economic growth. There may be several factors involved, including lower burden of malaria-related anemia, kidney damage, HIV, and other chronic diseases, and less wasted investment in education and training of people who would later die of malaria. Malaria may also raise birth rates. Because malaria disproportionately kills young children, causing about a quarter of deaths under age 5 years in endemic areas, parents may have extra children to ensure that some will survive. Parents might also invest less in educating each child because their resources must be spread among more children, some of whom may die. To reduce malaria, the WHO estimated that effective malaria prevention and treatment will need $2.5 billion per year in extra spending by 2007, and $4 billion per year by 2015. In 1998, WHO, UNICEF, UNDP (the UN Development Prgramme), and the World Bank began a campaign called Roll Back Malaria, to coordinate the approach to fighting malaria with the goal to halve the burden of malaria by 2010. The Global Fund to Fight AIDS, Tuberculosis and Malaria was set up later to raise and distribute money, and has pledged nearly $1 billion during the next 2 years to fight malaria. The money will support antimalarial actions thought to be most cost-effective, such as producing long-lasting insecticidal bed nets and providing effective antimalaria drugs such as artemesinin. The amounts raised so far are short of the goals. Jeffrey Sachs, now at Columbia University, estimates that one million lives per year could be saved by spending $2 billion to $3 billion on malaria, adding, "This is probably the best bargain on the planet." Sources: wikipedia.org, rbm.who.int How was this story's length set? Tsunami Devastates Some Indian Ocean CoastsBy Larry BaumOver 150,000 people were killed and over a million left homeless in the wake of a tsunami that swept outward from a huge, magnitude 9.0 earthquake off the northwest tip of Indonesia on 26 December. Indonesia's Aceh province was worst affected. The lack of a tsunami warning system in the region precluded evacuations that might have saved many of the lives that were lost. |
||
| How is Human News different? | Links | Contact Human News | |